Article by Dr Daniel Graham
Peripheral Neuropathy Awareness Week is an annual event observed primarily throughout the continental United States during the first full week of May.
This year, it runs from May 5 to 11 and essentially serves as a promotional campaign to increase awareness of peripheral neuropathy, its symptoms, causes, diagnosis and current treatments.
Peripheral neuropathy, also known as neuropathy, is a general term that describes many conditions that result from damage to the peripheral nervous system and is estimated to affect more than 20 million persons in the United States and some 190 million worldwide.
The purpose of this article is to provide a fairly comprehensive overview of peripheral neuropathy and to increase the knowledge of and education about this common and potentially crippling neurological disorder.
The body’s nervous system consists of two parts, the central nervous system (CNS), which comprises the brain and spinal cord, and the peripheral nervous system (PNS) – a network of nerves that relay information from the CNS to the peripheral parts of the body (arms, hands, legs, feet, internal organs, joints).

Peripheral neuropathy (PN) can affect multiple nerves (polyneuropathy), only one nerve (mononeuropathy) or many individual nerves sequentially (mononeuropathy multiplex).
Because peripheral nerves can react in only a limited number of ways to disease, polyneuropathies of many different origins may present with similar symptoms and signs. Indeed, most patients with polyneuropathy first present with a combination of sensory and motor symptoms and signs in the feet and lower legs, which later spread proximally (upwards) in the legs and gradually, over time involve the hands and forearms.
Despite the many similarities, a neuromuscular disease physician/neurologist can always limit the list of possible underlying causes of a polyneuropathy by determining the answers to several key questions: What is the temporal course of the polyneuropathy (acute, subacute, chronic, progressive, stepwise, relapsing/remitting)? Which nerve fibre types are involved (motor, large sensory, small sensory, autonomic)? What is the pattern of the polyneuropathy? Is there a family history of polyneuropathy? Is there a history of medical illness or are there signs suggesting a medical illness associated with polyneuropathy? Is there any history of occupational or toxic exposure to agents associated with polyneuropathy?
The answer to each of these questions is critical in the evaluation of patients with suspected polyneuropathy.
When a nerve is diseased, it can react in a limited number of ways. Consequently, many peripheral nerve disorders present with similar symptoms despite vastly different aetiologies (causes). Determining which nerve fibre types are involved has important diagnostic implications.
The overall pattern of polyneuropathy is determined from a detailed history and the clinical neurological examination, supplemented and confirmed by electrophysiologic/electrodiagnostic studies. In most polyneuropathies, there is a distal-to-proximal gradient of symptoms and signs. The longest nerves are most affected, resulting in a stocking-glove distribution of symptoms. Patients initially develop numbness or weakness of the toes and feet which then slowly progresses up the leg.
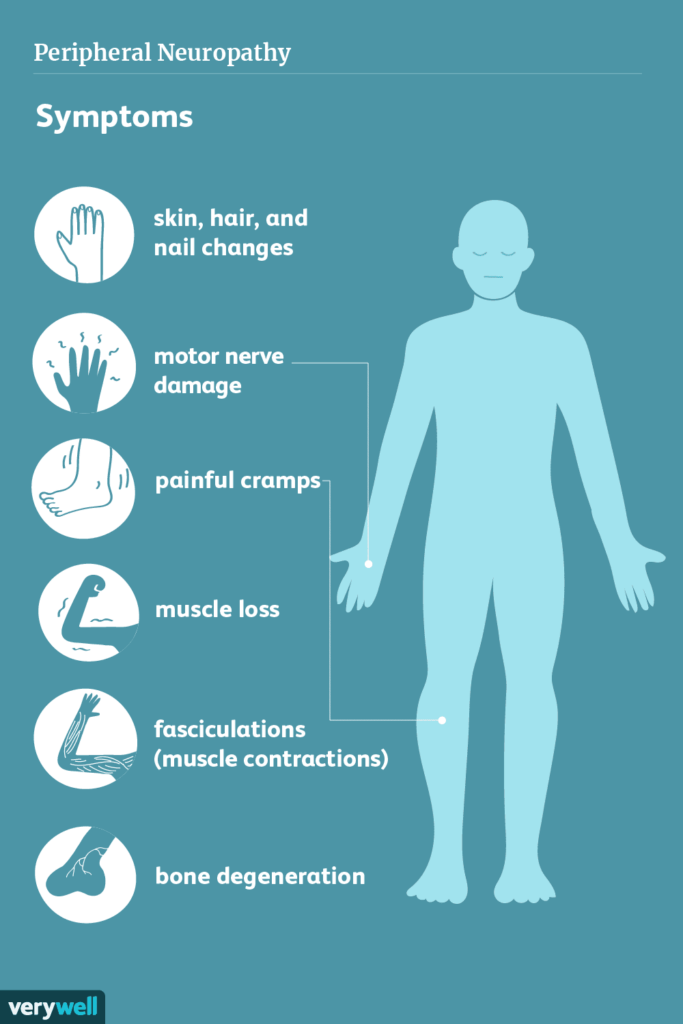
The symptoms of peripheral neuropathy may depend on the type of peripheral nerves that have been damaged.
There are three types of peripheral nerves: motor, sensory and autonomic. Some neuropathies affect all three types of nerves, while others involve only one or two.
Motor nerves relay impulses from the brain and spinal cord to all the muscles in the body. Sensory nerves convey sensations such as pain, temperature, vibration or touch from the skin and autonomic nerves regulate involuntary physiologic processes such as blood pressure, heart rate, sweating, respiration and digestion.
Symptoms of peripheral neuropathy often include:
- gradual onset of numbness, tingling, pins and needles, burning in the feet which may spread upward in the legs and later involve the hands
- a sensation of wearing invisible gloves or socks
- sharp, shooting, jabbing or electric-like pain in the legs
- loss of balance and coordination
- muscle weakness.
If autonomic nerves are affected, symptoms might include:
- excessive sweating or lack of sweating
- bowel, bladder or digestive problems
- drops in blood pressure causing dizziness or lightheadedness.
There are many causes of peripheral neuropathy including diabetes, infections, inflammatory and auto-immune disorders, vitamin deficiencies, chronic alcoholism, poor nutrition, traumatic or compression injuries, hereditary diseases, exposure to toxic substances and neurotoxic medications, especially those used to treat cancer (chemotherapy-induced neuropathy/CIN).
Distal symmetric polyneuropathies (DSPN) are the most frequent peripheral neuropathies, often representing long-term complications of systemic diseases such as diabetes, with the latter (diabetes) being the most common cause. In some cases, however, even with extensive evaluation, the causes of peripheral neuropathy in some persons remain unknown (idiopathic neuropathy).
The diagnostic workup in patients with suspected peripheral neuropathy includes a very thorough, detailed medical history, including family and occupational history followed by a detailed physical and neurological examination.
Electrophysiologic studies represent the current diagnostic gold standard in the evaluation of peripheral neuropathies assessing motor and sensory peripheral nerves in upper and/or lower extremities. Needle electromyography, a test that evaluates and records the electrical activity produced by a skeletal muscle, provides critical information about a host of neuromuscular disorders. Results from these diagnostic tests often allow for the differentiation between acute and chronic, focal and non-focal, or neuropathies affecting the core of the nerve fibre (axon) or its covering (myelin).
A very important, frequently unrecognized neuropathy is known as hereditary transthyretin amyloidosis with polyneuropathy (hATTR-PN), a rapidly progressive, debilitating sensory-motor polyneuropathy. Whilst it can impact all ethnic groups, certain racial groups, most notably people of African and Portuguese descent, have higher rates of the disease. Transthyretin (TTR) is a normal protein that through gene mutation or aging of the protein can become unstable and aggregate into insoluble fibrils called TTR amyloid. TTR-related amyloidosis is an underdiagnosed disease that mainly affects cardiac (heart) muscle and peripheral nerves and can be fatal if not treated on time.
Carpal tunnel syndrome (CTS), the most common of the entrapment/compression neuropathies (due to median nerve entrapment at the wrist) has recently been recognized as an early, even if non-specific, manifestation of hATTR-PN. In very recent studies, groups of researchers reported that CTS occurred in up to two-thirds of patients with hATTR-PN, and, more importantly, it may predate the diagnosis of hATTR-PN by up to ten years.

Their findings support the concept that carpal tunnel syndrome should be considered a ‘red flag’ for diagnosis of hATTR-PN especially when it occurs in both hands, has an early onset without risk factors (such as hand working activities), there is a positive family history and/or is severe or recurrent. Severe cardiac involvement may occur in the late-onset subtype, due to infiltrative deposition of the abnormal amyloid protein in the muscle of the heart (myocardium).
Such patients are at risk for sudden death due to heart failure (restrictive cardiomyopathy). The question of who should be screened is currently unanswered, but it has been suggested that nerve conduction studies in all four limbs, including studies of the median nerves be performed in ‘high risk’ persons.
Nerve conduction studies can distinguish patients who present with an acquired chronic polyneuropathy (e.g. chronic inflammatory demyelinating polyneuropathy/CIDP), from an inherited neuropathy (e.g. hereditary motor sensory neuropathy/HMSN). CIDP is an important diagnosis to recognize because a number of immunosuppressive therapies exist which can effectively treat this potentially disabling polyneuropathy.
Peripheral neuropathies represent a spectrum of diseases with different causes and are among the most common neurological disorders with an incidence of 77/100,000 inhabitants per year. A thorough workup, including detailed clinical history and examination, electrophysiological studies and comprehensive laboratory tests is warranted to identify treatable causes.







Comments