

By Dennis A Minott
The over six-year closure of Cornwall Regional Hospital (CRH) has had far-reaching effects on the Western Region of Jamaica, which relies on this facility as previously the only Type A hospital serving the area.
The closure, while necessary to address critical repairs, has created significant challenges in multiple areas. Here are the likely impacts:
1. Health Outcomes for the Population
The prolonged closure of CRH has had severe consequences for health outcomes in the region. A Type A hospital is vital for handling the most complex cases, including emergency surgery, intensive care, and specialized treatments. Without access to this level of care:
- Increased Mortality and Morbidity: Many patients requiring critical or specialized care have had to rely on smaller, less equipped facilities or travel long distances to the nearest functional Type A hospital, usually in Kingston and recently Falmouth. This delay in access to proper treatment could contribute to higher rates of mortality and morbidity, particularly in cases involving trauma, heart disease, stroke, and other critical conditions.
- Delayed Diagnoses and Treatments: With CRH closed, routine diagnostic procedures and treatment for chronic conditions have likely been delayed or diverted to smaller facilities with less specialized equipment and staff. This would have led to worsened health outcomes for patients with non-emergency but still serious conditions, such as cancer, diabetes, or hypertension.
- Limited Access to Emergency Services: The closure meant that patients in urgent need of emergency care, including those with trauma or life-threatening conditions, would have had to be transferred to other hospitals. The delays associated with such transfers can mean poorer outcomes, particularly for conditions like heart attacks, strokes, or severe injuries.

2. Employment of Health and Ancillary Workers
The closure of CRH has disrupted the employment of health and ancillary workers, which has likely created both direct and indirect social and economic challenges in the region:
- Job Losses or Reallocation: Many healthcare workers, from doctors and nurses to cleaners, security staff, and administrators, were either reassigned to other hospitals or faced furloughs or job losses. This created uncertainty for hundreds of employees who depended on the hospital for their livelihoods.
- Morale and Burnout: Those who remained employed but were transferred to other hospitals likely faced increased workloads in already strained facilities. For healthcare workers, this increased pressure without adequate support or resources can lead to burnout, reduced morale, and even departures from the profession.
- Loss of Training Opportunities: With a hospital of CRH’s stature closed, junior doctors, nurses, and other healthcare professionals lost out on valuable opportunities for hands-on training and experience in a major hospital setting. This loss is especially felt in specialized areas of medicine and surgery that require experience in high-volume, complex cases.
3. Cost of Treatment for the Indigent
The closure of CRH also had an impact on the cost of treatment for Jamaica’s most vulnerable population:
- Increased Financial Burden: Indigent patients who would have received treatment at CRH were often forced to seek care elsewhere, which in many cases meant more expensive private hospitals or longer journeys to government-run hospitals in other regions. Travel expenses, longer wait times, and the need for specialized care often led to higher costs, making it harder for the indigent to access timely and appropriate treatment.
- Strain on Other Healthcare Facilities: Other hospitals, such as the Savannah-la-Mar Hospital and the Falmouth Hospital, were forced to shoulder the added burden of emergency cases. However, these facilities did not have the same level of equipment, specialized staff, or resources as CRH, leading to the potential for poorer quality of care and increased fatalities.

4. Availability of Emergency Services
The closure of CRH directly affected emergency services in the Western Region:
- Longer Response Times: As the region’s only Type A hospital, CRH was a hub for trauma and emergency care. With it out of commission, patients requiring urgent care had to be diverted to other hospitals, often facing long waiting times. This delay in receiving timely emergency treatment is especially critical in cases like accidents, heart attacks, or strokes, where every minute counts.
- Limited Capacity in Other Hospitals: Hospitals like the Savannah-la-Mar Hospital and the Falmouth Hospital were forced to shoulder the added burden of emergency cases. However, these facilities did not have the same level of equipment, specialized staff, or resources as CRH, leading to the potential for poorer quality of emergency care and increased fatalities. Many a patient died needlessly.
5. Education and Training of Health Workers
The closure also impacted the education and training of healthcare professionals in the region:
- Loss of Clinical Training Opportunities: Cornwall Regional Hospital was an important training ground for medical students, nurses, and allied health professionals in Western Jamaica. With the closure, students and interns were forced to seek training placements at smaller, less equipped hospitals. This limited their exposure to the variety of cases and hands-on experience that would have been available at a major hospital.
- Loss of Research Opportunities: Hospitals like CRH play an important role in medical research, especially in underserved areas. With the hospital closed, opportunities for research, data collection, and collaboration with universities or international health organizations have been curtailed, which has broader implications for advancing medical knowledge and improving healthcare practices in Jamaica.

6. Broader Economic Impacts
- Tourism and Regional Development: Western Jamaica, a major tourist hub, also suffered indirectly from the closure of CRH. International tourists, local visitors, and even foreign workers in the region are likely to have felt a diminished sense of security regarding emergency healthcare availability. This could have influenced both the attractiveness of the region as a tourist destination and the willingness of foreign investors to establish businesses in the area.
- Impact on Social Infrastructure: Beyond health, the prolonged closure of CRH likely resulted in increased strain on other aspects of social infrastructure, from transportation networks (due to the need for patients to be transferred to more distant hospitals) to local economies that relied on the hospital as a major employer.
7. Long-Term Consequences
Looking ahead, the long-term consequences of the closure of CRH might include:
- Health System Strain: If the hospital’s repairs are not completed swiftly, there could be a long-term reduction in the region’s overall health service capacity, with poorer health outcomes becoming more pronounced over time, especially in the wake of emergencies, the COVID-19 pandemic, or any other future public health crises.
- Public Trust in Government: The failure to complete repairs in a timely and cost-effective manner may further erode public trust in the Jamaican government’s ability to manage critical public infrastructure projects. As healthcare is a basic human right, the perceived neglect of Cornwall Regional Hospital may fuel frustration and distrust among the population, particularly in the Western Region.
In summary, the closure of CRH has likely spawned a range of detrimental effects, including worsened health outcomes, loss of employment, increased costs for the indigent, reduced access to emergency services, and stunted educational opportunities for healthcare workers. All of this underscores the urgent need for effective and timely management of public health infrastructure projects, particularly for hospitals serving underserved regions.

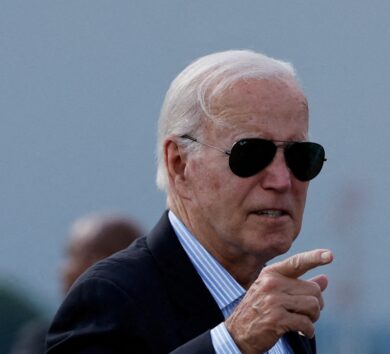
Dr Chris Tufton takes a cavalier approach
The long-serving Minister of Health’s recent declaration that “all’s well that ends well” in relation to the long-awaited reopening of Cornwall Regional Hospital (CRH) possibly in 2025 is, at best, a tone-deaf attempt to sweep under the rug the scale of mismanagement and neglect that has plagued the project for over six years.
To reduce such a catastrophic failure in governance to a trite Shakespearean platitude insults the intelligence of the Jamaican people, who have witnessed the untold suffering caused by this debacle.
“All’s well that ends well” might be comforting if this were a minor inconvenience or a routine hiccup in the healthcare system. But this is not the case. For over half a decade, the people of Jamaica’s western region, already facing significant healthcare challenges, have been forced to endure a stark absence of critical medical services, while political and bureaucratic inefficiency compound the already dire situation.
Thousands of citizens—many of them vulnerable, indigent, and in urgent need of specialized care—have been neglected. Health professionals, too, were displaced or forced to work under impossible conditions in understaffed and underfunded institutions. The economic, social, and emotional toll has been immense.
The minister’s cavalier dismissal of the problem under the guise of an eventual resolution fails to address the systemic failures that allowed this crisis to unfold in the first place. Far from an “end” that justifies the means, this closure has exposed glaring weaknesses in leadership, project management, and financial oversight. It has also highlighted the deep inequality in the allocation of resources and the dismal treatment of healthcare workers who were left without adequate support.
The time has come to hold those responsible to account. I repeat my call for a full Judicial Commission of Inquiry into the CRH disaster. This inquiry should not merely probe the mishandling of the repairs or the mounting costs, but also examine the deeper governance failures that allowed this crisis in our health system to fester. The proposed commission must investigate the political, bureaucratic, and technical failings, and it should offer concrete recommendations to prevent such a scandal from occurring in the future.
Jamaica deserves more than platitudes and empty assurances. It deserves accountability, transparency, and, most importantly, a healthcare system that serves its citizens with the empathy, respect, and urgency they deserve. “All’s well that ends well” may be a nice soundbite, but it is no substitute for genuine reform and a reckoning with this catastrophic failure.





Comments