

In his sectoral presentation to Parliament, Chris Tufton, Minister of Health and Wellness, remarked that the health of Jamaicans is certainly better today than nine years ago. Tufton continued that while he felt the current health system is not where it should be, his speech would demonstrate why he felt that statement was true and asked Jamaicans to stay the course so that this Government can continue to build our health system.
Policy success: Shift to health centres
Over the last year, the public health system saw some 3,046,946 visits; 1,892,106 to health centres and 1,154,840 to hospitals. It is important to note that more Jamaicans are visiting their health centres, and less to our hospitals, when compared to five years ago. This is an important policy success!
There were approximately 300,000 more visits to health centres and 250,000 less visits to hospitals in 2024. This is so because our health centres have benefited significantly from improvements in infrastructure, added services and better service delivery.
This Government has invested in community healthcare and the people are getting the benefits of this improved service. I will demonstrate why.
To provide context, in 2024, there were 63,562 surgeries performed; 15,392 major surgeries, 11,743 minor surgeries, 7,120 day surgeries and 29,301 minor outpatient surgeries.

Some 10,097,052 lab tests were done; 9,651,083 in hospitals and 445,969 in health centres. There were 703,780 diagnostic (imaging) tests done. There were 511,791 visits to the Accident and Emergency.
These are not just numbers; these are people who benefit from the system in 2024.
Together, more than 2,400 doctors, some 5,500 nurses, 2,000-plus community health aides, more than 1,900 paramedical and allied healthcare workers as well as our administrators, and contractors of services like catering, cleaning and portering, security personnel, direct and indirect staff, work daily to get the job done.
We recognise them and we should celebrate their efforts and sacrifice, even as we continue to work to improve on the areas that require improvement.
Opposition comments

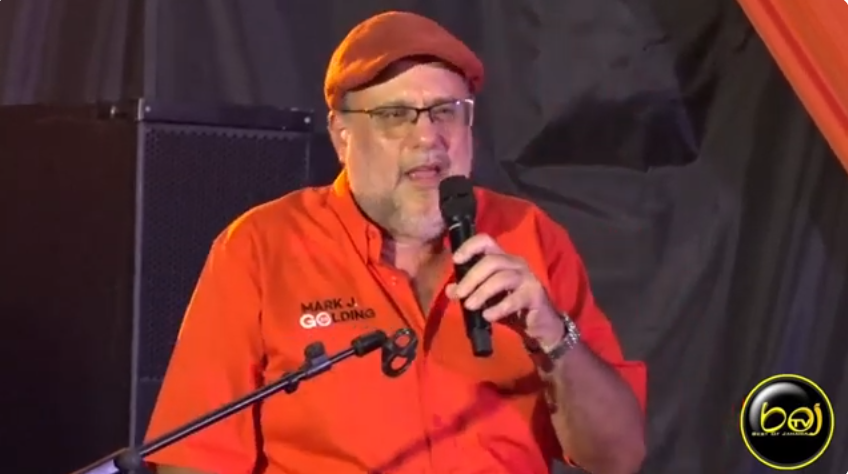
The Opposition would like the Jamaican people to believe that they, finally, in 2025, have the answers to the challenges in public health.
They frame their conversation in isolation of the context of where we are coming from, where we are now after nine years as Government, and the vision and plans we have for the future, as reflected in our ten-year strategic plan for health, tabled in 2018. They also conveniently ignore current plans being implemented to improve the system after decades of neglect.
It’s a self-serving, deceptive and dishonest narrative.
I urge us to cast our minds back to 2015, and just look at how they left the health system; simply put – BROKEN. The news headlines tell the tales of woe and despair.
Madam Speaker, having cast our minds back to 2015 as a base year for an objective comparison, I would also say that we should not go by media headlines alone. Headlines do not tell the whole story. Let us also consider the hard facts.
More money for health

Back in 2016/17, the budget for capital projects in health was J$1.88 billion while the staffing budget was J$31.12 billion.
This year, 2025/26, Health’s budget for capital projects is up to J$10.18 billion, a more than five-fold increase from 2015, and from $6.93 billion in the last financial year (2024/25).
The staffing budget stands at $93.77 billion, up from $33.82 billion in 2016/17!
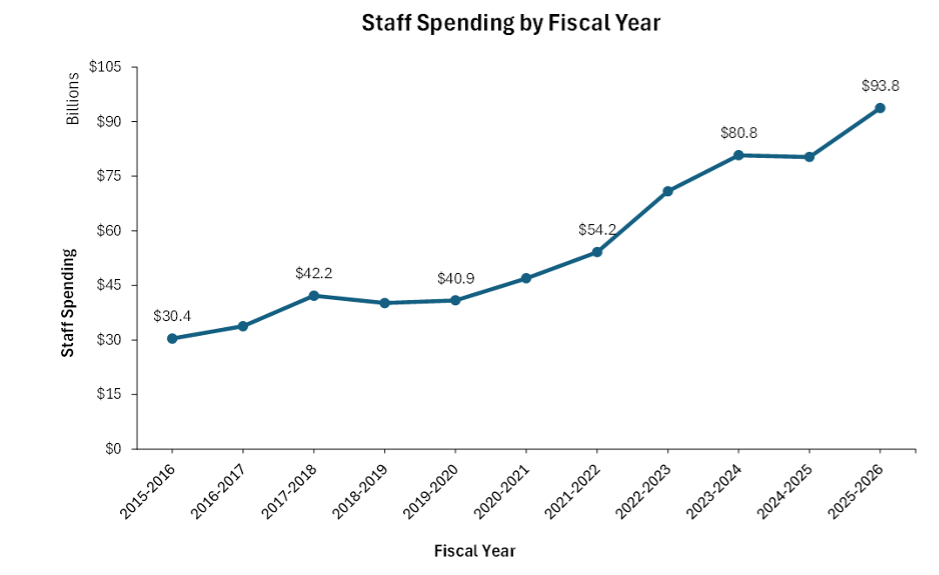
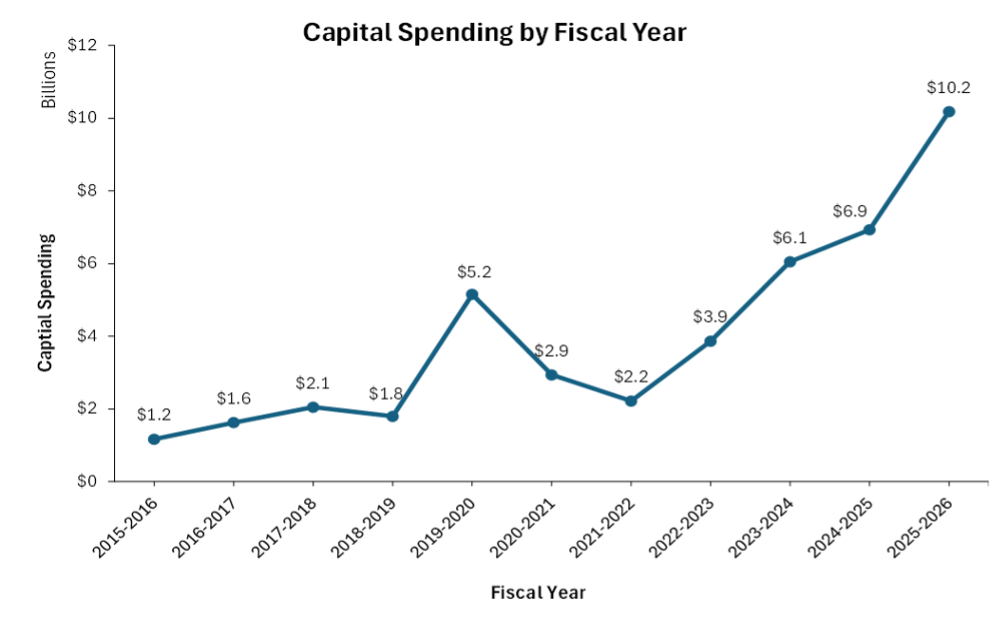
Simply put, under this Government’s tenure, there have been more hospitals and health centre buildouts, more posts for healthcare workers, and more compensation for our workers!
Madam Speaker, there can be no question that this Administration is making a sincere and tangible attempt to improve our public health services and certainly better than any attempt before 2015.
There are still challenges, but we are better off than we were back in 2015. We must stay the course!
More services through the NHF
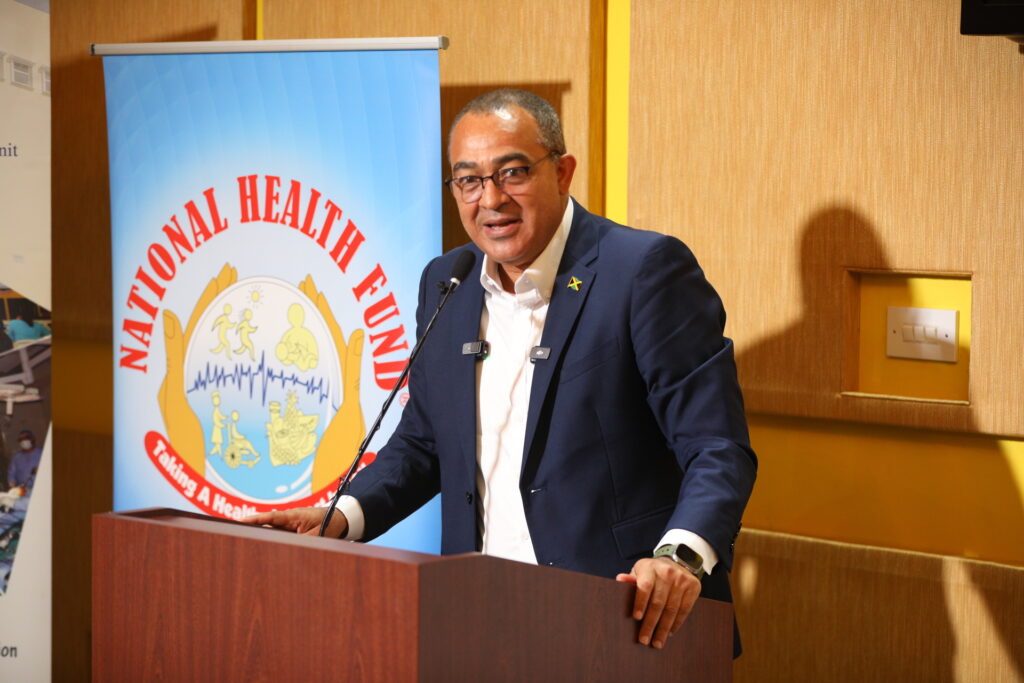
Madam Speaker, another example of how and why the Jamaican people are benefiting more from Government health services since 2015, is through the expanded role of the National Health Fund (NHF).
In 2015, there were limited programmes to address the prevailing issues in health. The National Health Fund (NHF), over the past nine years, has expanded significantly to support Jamaicans.
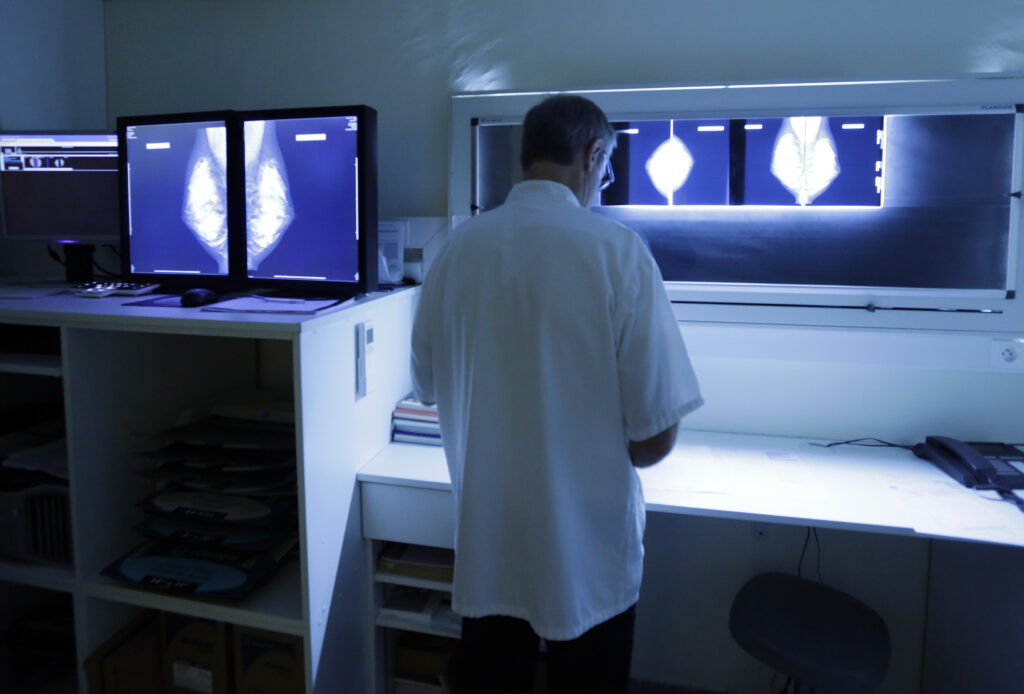
One significant example is the NHF’s provision of coverage for only two cancers in 2015 – breast cancer and prostate cancer. Today, the NHF provides coverage for five cancers; lung cancer, colorectal cancer and multiple myeloma, in addition to breast cancer and prostate cancer.
Madam Speaker, it is important to note that the subsidy for breast cancer receptor studies has increased from $4,800 to $12,500, even as we have introduced a $1,300-subsidy for pap smears for women ages 21 to 64.
And our men have not been left behind. Today, we have also expanded the $1,600 subsidy for PSA tests to include men ages 40-75.
Further, the agency has also expanded its coverage from some 16 conditions in 2015/16 to 24 conditions in 2024, including Attention Deficit Hyperactive Disorder, Lupus, Parkinson’s Disease and Thyroid Disease.
To punctuate the point, Madam Speaker, the NHF last year filled nearly three million prescriptions for Jamaicans compared to less than one million in 2015!
- In 2015/2016, the NHF spent $3.66 billion on drugs dispensed through its Pharmacy Services Division, which oversees 106 Drug Serv pharmacies across the island.
- This figure increased to $9.81 billion in 2024/25.
- The total drug expenditure over the period from 2015/2016 to 2024/2025 amounts to $64.98 billion.
We are better off today than we were in 2015! We must stay the course!
Debunking myths
The Leader of the Opposition says he wants to improve primary care, with a focus on building out health centres. This is a good thought, but has he made any effort to see what we have been doing?
Madam Speaker, last year we published and tabled here in this House a new model for Primary Healthcare. I invite the Opposition Leader and his team to meet with me and my team to further understand and, where necessary, collaborate.
This published 10-year Primary Health Care Reform Plan for Jamaica outlines a clear shift towards screening and prevention and we are doing this in a number of ways.
More services
We are adding more services at the community or primary level, including adolescent health and elderly health, rehabilitative and palliative care, as well as ophthalmological and audiometric screening – together with dentistry, diabetic retinopathy, and laboratory services, among others.
Madame Speaker, it is not by chance that we are getting more visits to our health centres. We must stay the course!
Physical & ICT Upgrades

We are also improving the physical and information, communication and technology infrastructure at health centres. The most significant buildout is taking place through a collaboration among the Government of Jamaica (GOJ), the Inter-American Development Bank (IDB) and the European Union (EU), with the implementation of the Health System Strengthening Programme (HSSP).
Madam Speaker, under the HSSP, we are building out 13 health centres and hospitals, equipping them with fully digitised patient records and modern diagnostics machinery. These facilities will see new services and expanded staff for the communities they serve.
TABLE: HSSP benefitting facilities
| Facility | Estimate (USD) | Estimate (JMD) |
| Spanish Town Hospital | 35,500,000 | 5,609,000,000 |
| May Pen Hospital | 2,626,045 | 414,915,110 |
| St. Ann’s Bay Hospital | 3,995,000 | 631,210,000 |
| May Pen West Health | 1,930,662.34 | 305,044,649.72 |
| May Pen East Health Centre | 4,734,642.86 | 748,073,571.88 |
| Chapelton Community Hospital | 672,454.55 | 106,247,818.9 |
| St. Ann’s Bay Health Centre | 1,960,922.08 | 309,825,688.64 |
| Ocho Rios health Centre | 4,808,504.40 | 759,743,695.2 |
| Brown’s Town Health Centre | 4,845,310.26 | 765,559,021.08 |
| Mocho Health Centre | 1,236,590.91 | 195,381,363.78 |
| Greater Portmore Health Centre | 3,251,332 | 513,710,456 |
| Old Harbour Health Centre | 4,313,360 | 681,510,880 |
| St. Jago Park Health Centre | 3,271,548 | 516,904,584 |
| Total | 73,146,372.84 | 11,557,126,908.72 |
These figures represent one programme.
Under Operation Refresh, we have completed 13 health centres to the tune of more than $100 million ($105,739,666.47). The works have included the addition of AC units, waiting area upgrades, doctors’ offices, bathrooms and the addition of running water, as well as kitchenettes.
In fact, Madam Speaker, in the last five years, this Administration has upgraded 138 additional health centres to the tune of $3.88 billion across the four health regions.
TABLE: REGIONAL SPEND ON HEALTH CENTRES
| REGION | SPEND (JMD) | |
| WRHA | Westmoreland Trelawny St James Hanover | 99,338,111.2 87,652,016 205,220,204 49,334,149.5 |
| SRHA | Clarendon Manchester St. Elizabeth | 98,893,829.2 318,216,990 621,036,923 |
| NERHA | St. Mary Portland St. Ann | 355,920,230 515,306,915 1,134,475,139 |
| SERHA | Kingston St. Thomas St. Catherine | 214,905,752 141,805,006 46,126,858 |
| TOTAL | $3,888,232,123.2 |
In addition to a range of service offerings at the new CRH, we will also engage a maintenance arrangement to ensure that the hospital is never again faced with the neglect of the past. This, Madam Speaker, is progress. We must stay the course!
Kingston Public Hospital

We need to avoid a second CRH. As a Government, we are, therefore, now focusing on the Kingston Public Hospital (KPH). The facility, which opened its doors in 1776 and which currently boasts 484 beds, has been plagued by challenges due to the age of the plant and poor maintenance.
I am happy to announce that we have now identified lands for lease to purchase and have commenced plans for a new KPH.
Madam Speaker, a Land Use Survey Report was prepared on the properties around KPH, inclusive of the 35 parcels identified. The National Land Agency is coordinating the compulsory acquisition of the required lands.
Other capital projects

Madam Speaker, significant renovations are also taking place at other health facilities across the country, among them the University Hospital of the West Indies.
That process, Madam Speaker, is now in the final stages of procurement and will see the construction of a new 6-storey building, 120,000 square feet medical facility, which will accommodate an additional 40 medical and surgical beds; improvement to outpatient or ambulatory surgery, lecture rooms and conference rooms. Also included in the UHWI project is the upgrade of the cardiology hybrid interventional surgery room and the neonatal intensive care and administrative departments.
Together with Western Child & Adolescent Hospital (220 beds), which is in its final stages of completion, these developments should see the island with more than 450 additional beds (129 – Spanish Town Hospital; 40 – UHWI; 8 – St. Ann’s Bay Regional, 32 – Chapleton Health Centre; and 30 – Cornwall Regional) – this in addition to the 384 beds added over the last five years, including COVID wards.
Madam Speaker, we not only have a plan, the plan is being implemented! We must stay the course!
A new HR push
Madam Speaker, a critical pivot point to improve health services is filling the gaps that exist for healthcare workers.
We have long had shortages of specialist nurses, specialist doctors and other critical support staff like radiologists and biomedical engineers. Our last count suggests a shortage of, for example, radiologists by more than 50 per cent and a shortage of some 1,388 of specialist nurses
Two factors contribute to this. The increasing mobility of our skilled labour force, with the increasingly attractive offers to incentivise economic migration.
Secondly, the Government’s health reform strategies which are seeing more posts and a greater demand for these specialised skill sets locally.
Madam Speaker, we have to fix the HR issue if we are to see the service delivery gains from infrastructure expansion.
TABLE: STATUS OF SPECIALIST NURSES AS AT DECEMBER 2024
| Category of Specialist | Currently Employed | Current Needs | GAP |
| RN/Midwife | 385 | 697 | 385 |
| Emergency Nurse | 85 | 355 | 270 |
| Psychiatric Nurses | 140 | 360 | 220 |
| Paediatric Nurses | 69 | 283 | 214 |
| Critical Care | 200 | 394 | 194 |
| Operating Theatre | 112 | 275 | 163 |
| Neonatology | 70 | 222 | 152 |
| Oncology | 21 | 130 | 110 |
| Orthopaedics | 0 | 104 | 104 |
| Burns | 0 | 84 | 84 |
| Nephrology | 59 | 130 | 71 |
| Wound Care | 0 | 69 | 69 |
| Cardiac | 2 | 70 | 68 |
| Ophthalmology | 2 | 54 | 54 |
| Total | 1,108 | 2,496 | 1,388 |
Madam Speaker, we have to be more aggressive in our push to right size our HR policy for better service delivery.
Firstly, if Jamaicans are qualified and available, we will pursue this option as a priority. We also have to help locals who are willing and able to qualify for these posts. We are doing just that.
Our decision to introduce the Barry Wint Scholarship last year is a demonstration of our preference for Jamaicans to fill these posts. Last year we offered more than 600 scholarship places under this programme, with 536 offers taken up.
TABLE: THE FIRST SCHOLARSHIP RECIPIENTS
| Areas of Study | Count of Programme of Study Covered In 2024/2025 Intake | Total Value of Scholarship Payment (JMD) |
| MB; BS | 163 | 133,190,013.35 |
| BSc. Nursing | 161 | 80,423,020.52 |
| Doctor of Dental Surgery | 49 | 46,570,350.00 |
| BSc. Social Work | 23 | 5,700,658.70 |
| BSc. Diagnostic Imaging (Radiography) | 17 | 12,924,000.00 |
| BSc. Environmental Health | 16 | 7,557,310.00 |
| Doctor of Pharmacy | 16 | 15,173,266.50 |
| MSc. Public Health (General) | 13 | 9,856,500.00 |
| BSc. Midwifery | 11 | 4,647,260.00 |
| BSc. Medical Technology | 6 | 2,132,830.00 |
| BSc. Biomedical Engineering | 5 | 5,000,000.00 |
| BSc. Pharmacy | 5 | 2,365,870.00 |
| Doctor of Public Health | 5 | 3,981,600.00 |
| MSc. Health Administration | 4 | 2,000,000.00 |
| MSc. Public Health (Nursing) | 4 | 2,820,417.00 |
| Associate Degree in Health Information Technology | 3 | 1,479,100.00 |
| BSc. Physical Therapy | 3 | 519,799.50 |
| MBA Health Care Management | 3 | 1,000,000.00 |
| Medical Technology | 3 | 1,294,010.00 |
| Certificate in Critical Care Nursing | 2 | 1,114,400.00 |
| MSc. Global Health | 2 | 1,000,000.00 |
| MSc. Social Work | 2 | 862,931.00 |
| BA. Electrical & Computing Engineering | 1 | 480,180.00 |
| BSc. Dental Laboratory | 1 | 578,190.00 |
| BSc. Dietetics/Nutrition | 1 | 292,800.00 |
| BSc. Health Science | 1 | 314,450.00 |
| BSc. Occupational Health and Safety | 1 | 457,600.00 |
| BSc. Pharmaceutical Tech. | 1 | 571,020.00 |
| BSc. Software Engineering | 1 | 173,266.50 |
| DBA | 1 | 958,632.30 |
| Dip. Animal Health Production and Veterinary Public Health | 1 | 1,000,000.00 |
| MPh. Nutrition | 1 | 304,209.00 |
| MSc. Advance Nursing Education | 1 | 1,000,000.00 |
| MSc. Counselling Psychology | 1 | 932,808.00 |
| MSc. International Public Health | 1 | 491,245.80 |
| MSc. Medical Physics | 1 | 360,000.00 |
| MSc. Nurse Anaesthesia | 1 | 1,000,000.00 |
| MSc. Nursing Administration | 1 | 1,000,000.00 |
| MSc. Nursing Anaesthesia | 1 | 1,000,000.00 |
| MSc. Physical Education and Sports Management | 1 | 1,000,000.00 |
| MSc. Public Administration | 1 | 1,000,000.00 |
| MSc. Renal Medicine | 1 | 1,000,000.00 |
| Grand Total | 536 | 355,527,738.17 |
NEW SCHOLARSHIP ANNOUNCEMENT
Madam Speaker, this year we will award another $500 million, with advertisements to be placed in our print media and on the Ministry’s website beginning this week. It is important to note that these scholarships will be targeted to areas where we have shortages and are trying to fill gaps in our HR requirements.
As such, this year’s scholarship offering will favour persons who are pursuing studies in biomedical engineering, medical physics, occupational therapy, radiation therapy and dental nurse therapy, in addition to third- and fourth-year nursing students.
TABLE: Areas of focus for new recipients
- Biomedical Engineering
- Medical Physics
- Speech Therapy 3rd – 4th year Nursing and
- Midwifery
- Occupational Therapy
- Radiation Therapy
- Dental Nurse Therapy
- Nurse Educators
By our calculations, the Barry Wint Scholarship Programme is, by 2027, to have yielded 63 nursing graduates, four (4) biomedical engineers, three (3) social workers and 15 diagnostic imaging professionals who will serve the public health system. By 2028, the programme is to see the addition of 56 Nurses; 10 Midwives; and nine (9) Social Workers trained to serve the public health system. By 2029, the programme is to see the addition of 134 Doctors and 42 Dentists.
We are also given priority to locals who are currently qualified through our first career expo in January of this year. During the two-day event, close to 10,000 Jamaicans converged on the University of the West Indies, Mona to see displays and receive information on careers in public health.
We also, through our job fair, received some 2,087 applications, with 340 invited for assessment and 294 shortlisted. Some 124 interviews were done and my latest report from the Regional Health Authorities and the Ministry’s Human Resources Department indicates that 53 were offered posts.
Policy alignment to HR needs

Madam Speaker, our HR policy gives Jamaicans priority at all times. But history has shown that there is a limit to this due to external and local factors. We have to continue to expand our reach to meet the demands of our healthcare needs.
This is not new. We are committed to continuing our Cuban partnership as these arrangements have been of significant benefit over the years. We currently have 88 Cuban doctors and 199 nurses here. I want to commend our Cuban healthcare team members, without whom we would find it very difficult to serve Jamaicans in hospitals.
That programme, too, has evolved. For example, over the last year, the Cuban Eye Care programme saw more than 18,000 (18,109) cases in consultation while some 1,232 surgeries were done. There were 811 Cataract, 418 Pterygium and three minor surgeries, such as for a cyst in the eye or other growth.
Some 605 retina laser treatments were performed under the programme, as well as 391 anterior retina laser and 24 ocular ultrasounds.
Madam Speaker, the future of HR in health will require more collaboration, using technology and friendships to fill the gaps that have been and are being created from a highly mobile labour force.
We have to look wider, think deeper and adjust our traditional thinking around the WHO and the HOW to get more skills in healthcare.
We have started through exploring long-term relationships in training and clinical exchanges with India, Philippines and Nigeria, in the first instance. These countries were targeted based on existing friendships, compatibility with language, training modules and technology availability, and past experiences with these nationals as healthcare workers in Jamaica.

Earlier this year, I visited India and the Philippines, and we are making progress. We have established MOUs with both countries and are now developing course outlines for joint training where we will share faculty and do clinical rotation in those jurisdictions, where possible.
We are also looking to deepen collaboration with Nigeria around human resources for health. Already, we have held meetings here in Jamaica with the yields including five volunteers coming to the island under the existing Technical Manpower Assistance Agreement. Two of the five volunteers are nurse educators and will be deployed to our in-service training unit to execute training of specialist nurses. The other three are specialist nurses who will serve elsewhere in the system.
At the same time, where shortages exist, particularly in the short term, we will also seek arrangements for clinical rotation of those nationals to fill the void. Currently, we are focusing on our specialist nurses together with categories of workers including biomedical engineers.
More tech
We are also looking at remote services using technology. One example is in the area of radiology. We have shortages of radiologists but we can outsource reading of the images with the right technology. We are currently discussing with our overseas partners this possibility.
Madam Speaker, we will, through various programmes, initiate training for 100 healthcare professionals over the next year. Over the next three years, we expect to engage at least 500 healthcare professionals to allow for the enhancement and expansion of service delivery.
Addressing pain points
Madam Speaker, despite our best efforts and the progress we have made, we have areas of our health services that we need to continue to improve on. In fact, we have areas where, with a bit more effort, at the Region and/or hospital levels, we can do better, and we need to do better. These are our ‘Pain Points’, or service delivery areas where client dissatisfaction is too high.
Operating theatres

We have 73 Operating Theatres in our public health system, including 17 at the University Hospital of the West Indies. At any given time, approximately 20% are down and, more often than not, unexpectedly so. This has contributed to delays in patient elective surgeries. It is also true that in a high-trauma society, elective surgeries are oftentimes rescheduled due to trauma cases coming in unexpectedly. We need to ensure better maintenance of our operating theatres and do better scheduling for trauma cases.
I have been assessing this issue with administrators and surgeons and have concluded that limited routine maintenance and in in-house capacity and less than adequate external supplier reliability are big parts of the challenge we face. We need to build capacity and have better planning in this area.
I have asked the Regional Health Authorities to move speedily to:
- appoint an Operating Theatre Manager at each hospital, whose responsibility it will be to ensure that best practice protocols are followed for scheduled maintenance and usage; and
- develop and implement a revised policy on supplier servicing and inventory of parts to ensure quick turnaround for repairs.
A major pain point in this area is maintaining air quality through efficient ventilation systems. I have asked that ALL OTs have a back-up ventilation system for when the main system goes down, either unexpectedly or for maintenance.
Madam Speaker, I am happy to announce that with the new build out of health infrastructure, we will add another 27 or 37 percent increase in new operating theatres, over the next two years.
Table: NEW OTs
| Facility | OT |
| Cornwall Regional Hospital | 11 |
| Spanish Town Hospital | 5 |
| St. Ann’s Bay Regional Hospital | 1 |
| May Pen Hospital | 1 |
| Western Child & Adolescent Hospital | 4 |
| Chapelton Community Hospital | 1 |
| Noel Holmes Hospital (Hanover) | 1 |
| National Chest Hospital | 1 |
| Lionel Town Community Hospital | 1 |
| Linstead Hospital | 1 |
We will improve our existing maintenance arrangements for our OTs and add significant inventory of new OTs over the next two years. Let’s stay the course!
Triaging of A&E Departments

Madam Speaker, as earlier noted, last year we saw 511,791 visits to our Accident and Emergency (A&Es) wards, up to 30 per cent of which could be seen at a health centre.
Many Jamaicans still do not understand that A&Es do not operate on a first-come, first-served basis, so that those cases that are not urgent are likely to be told to wait for many hours before seeing a doctor, following an initial assessment. They would understandably become disgruntled. We have to work harder to fix this.
Madam Speaker, in 2016, we started to extend the hours in health centres that were close to hospitals to receive the clients who could be seen in primary care after 4:00 pm. We started with the clinics and have since expanded. Twenty-nine (29) health centres now offer extended hours beyond 4:00 pm, some of them until 10:00 pm and some on weekends.
As part of the expansion of this initiative, named Extended Care, we will increase these numbers by 25 per cent over the next one year even as we extend the opening hours to 10:00 PM across participating facilities. We will also explore extended hours for pharmacy services.
This will allow persons who work during the day to visit the clinics for routine check-ups, screening and monitoring of chronic illnesses while providing an alternative to persons visiting the emergency departments and in so doing help to further reduce wait times while improving patient satisfaction levels.
TABLE: Health Centres presently offering extended hours
| Parish | Health centres with extended hours | TOTAL |
| St. Thomas | Morant Bay | 1 |
| KSA | Slipe Pen Road, Glen Vincent, Olympic Gardens, Duhaney Park, Windward Road, Harbour View, Stony Hill, Gordon Town | 8 |
| St. Catherine | St. Jago Park, Linstead, Greater Portmore, Waterford | 4 |
| Clarendon | May Pen Health, Spaulding, Chapelton Community Hospital | 3 |
| Manchester | Mandeville CHC | 1 |
| St. Elizabeth | Santa Cruz and Black River | 2 |
| Westmoreland | Savanna-la-Mar, Negril, Darliston, Whitehouse | 4 |
| St. James | Mt. Salem Changed to Type V with CRH Rehab | 1 |
| St. Ann | Alexandria Community Hospital St. Ann’s Bay and Ocho Rios | 3 |
| St. Mary | Highgate and Port Maria | 2 |
| Total | 29 |
In 2015, there were more than 300 primary care facilities but only 60 of these were offering Doctors’ consultations or Curative visits 5 days per week. This resulted in persons bypassing health centres, prompting crowding and long waiting times at hospitals or persons ignoring their illnesses to their detriment.
The Government of Jamaica is committed to further improve primary health care. Under the Primary Health Care Reform, we will therefore also increase the number of health centres offering access to doctors 5 days per week by more than 100%. This means we are targeting 67 health centres to be expanded over the next 3-5 years.
This expansion will allow clinics to move from having doctors at the health centres once or twice per week or once or twice per month, to having this full service 5 days per week.
To this end, we are partnering with the National Housing Trust to upgrade these facilities. Already for 2025/2026, five hundred million dollars have been allocated for infrastructure improvements. This partnership will continue over the next three to five years, reflecting another significant investment in and improvement of primary health care.
Hospital visitations

Madam Speaker, visits to hospitals by family members are currently very restricted and in many cases with good reason. Overcrowding and infrastructure limitations can create logistics challenges and compromise patient care. At the same time, there is tremendous value in allowing more family access to our patients for more time, under controlled circumstances.
It is therapeutic both for the patient and the concerned family member. Also, with the right protocols in place, family members can act as patient assistants to their loved ones, easing the burden on the attending nurse or nursing support. Reading to a patient, feeding them, just talking to them can be a valuable emotional and social service that can contribute to the healing process.
Madam Speaker, we will review our visitation policy to expand visitation hours in select circumstances and allow some tasks to be undertaken by family members as they contribute to the care of their loved ones.
I have asked the CMO to coordinate with RHAs to develop a new policy on patient visits with an implementation timeline of September 2025. We will start with our children wards at Bustamante Hospital for Children and, later, the Western Child & Adolescent Hospital.
Over the next several months, we will standardise the protocol for other facilities, including Princess Margaret Hospital, Percy Junor Hospital and Port Antonio Hospital.
Healthcare is about community and compassion; we must bring more hands on deck to support patients even at the secondary levels.
Food handlers permit

There are far too many complaints about the excessive wait times for Food Handlers Permits. More than 300,000 Jamaicans have to apply and reapply each year, sometimes waiting up to six months to go through the process. Madam Speaker, it is inefficient and supports non-compliance. We have to fix it.
Working with the team from the Environmental Health Division, we will overhaul and transform the National Food Handlers Training & Certification Programme.
As part of those efforts, we will:
- extend the term for a Food Handlers Permit renewal from one to two years;
- Introduce convenient bill payment service options, effective January 1, 2026;
- implement a bi-modal modular training format to reduce certification-processing time from three weeks to two weeks;
- introduce new technology to facilitate faster and more efficient processing to eliminate delays and backlogs;
- increase the cadre of professionally trained food handlers to reduce the risk of outbreaks linked to improper food handling; and
- increase application access points, reducing wait time and enhanced delivery process.
Pharmaceutical approvals

Madam Speaker, last year we saw 2,518 applications for approvals at the Standards and Regulations Division. Ten years ago, we were averaging 1,727 applications, which reflects an increase of 791 (46%) annually. Currently, 80% of dossiers submitted are delayed due to incomplete or incorrect information.
Manufacturers and importers have long complained about the long delays in getting a final response to their applications for drugs. There are several reasons for these delays, which are not always the fault of the Standards and Regulation Division. However, our lack of clarity and sometimes inefficiency in responding does create a credibility gap between the agency and the applicants. We have to fix this.
We will move, over the next year, to do the following policy changes, based on discussions with the team.
- Establish a protocol for greater dependence on the Reliance System for drug approvals, in collaboration with US, UK, and European standards. This means applicants who have already met these standards will be placed on a fast track for approvals, once they submit the appropriate documents.
- We will also move to digitise the application process so that applicants will not need to wait for a response to determine the incomplete nature of their application as these will be flagged in the online application while filling out forms. Currently, 80% of dossiers submitted are delayed due to incomplete information. Applicants must play their part in ensuring that the system works more efficiently.
- In addition, we will establish an express window for local manufacturers who apply for approvals once they are manufacturing locally for the local and export markets.
We will do this over the next year. We must stay the course!
Diagnostic testing

Despite the progress made in providing diagnostic equipment for public patients through acquiring new equipment for outsourcing, still too many Jamaicans have to wait for these tests.
Last year we did 703,780 imaging tests, and over the past year we have acquired 17 pieces of diagnostic equipment. Still, too many Jamaicans complain, particularly when they have to travel from the hospital to a private facility to get their tests done. We understand the inconvenience, and we are moving to fix this.
It is against this background that the Ministry is currently engaged in the acquisition of additional equipment. The Ministry is currently in the process of procuring 16 pieces of equipment, including 10 CT scanners and six MRI machines.
Last year, I outlined the new policy towards leasing of certain diagnostics equipment as opposed to purchasing with limited capacity to maintain, to benefit from ongoing servicing and renewal of the fleet to ensure optimal service delivery. I am happy to announce that we are close to implementing this policy.
At this time, we are progressing the procurement process.
School nutrition policy
Madam Speaker, we in public health are extremely happy that the School Nutrition Policy has been approved by the Cabinet. We think this could potentially be a game changer in the fight against early onset of NCDs in the lifecycle of a Jamaican.
While the implementation of this policy is being driven by the Ministry of Education, Skills, Youth, and Information, we will continue to offer full support and collaboration in its further implementation, through the development of dietary guidelines and training, using our nutrition department and our Executive Chef.
We will also continue our collaboration around our school’s mental health programme and our Jamaica Moves in schools initiative to keep our youngsters engaged in physical activities.
Electronic immunisation registry (EIR)

Madam Speaker, Jamaica has long maintained a strong immunisation programme, but to meet modern health demands and maximise impact, innovation is needed. The EIR pilot project, led by the Ministry of Health and Wellness, will be rolled out in the coming months and marks a bold step forward, a transformative shift from manual data entry to a fully digital immunisation system that supports real-time decision-making and system-wide improvements.
The healthcare system will benefit from real-time intelligence, integrated service delivery, patient empowerment, targeted interventions By identifying who is being missed, where, and why, the EIR enables data-driven, community-specific outreach that boosts coverage and equity and improved outcomes: Ultimately, the EIR will help achieve higher vaccine coverage, fewer missed doses, and better protection for all.
This is more than a system upgrade; it is a reimagining of how immunisation services are delivered. With the EIR, Jamaica is not just keeping pace with global health innovations; we are leading the way toward a smarter, more responsive, and more resilient healthcare future. It will make the immunisation process smarter, faster, and more efficient, strengthening the health system’s ability to protect every citizen through timely and effective vaccination.
Meanwhile, Madam Speaker, Jamaica has continued to distinguish itself with its immunisation coverage. In 2024, the island won the Henry C Smith Award for the most improved immunisation coverage in 2023. The award was announced at the 38th Caribbean Expanded Programme on Immunisation (EPI) Managers’ meeting held in St Kitts and Nevis in November 2024.
Since then, in 2024, we have continued to have high immunisation rates, achieving and surpassing the 95% target for all 8 antigens. In the face of declining immunisation rates in many countries and the outbreaks of vaccine-preventable diseases on the rise, this is a significant achievement for Jamaica and is a reflection of our strong primary care system.
Let us stay the course!
Our older persons

Madam Speaker, the older population (60 years and older) in Jamaica is the fastest growing age group, increasing at approximately 1.9 per cent annually from 264,772 to 364,200 between 2001 and 2030.
The dependent older person (65 years and older) was estimated at 199,478 (7.7%) in 2001 and is expected to increase to 321,664 (11.2%) in 2030. The working age will reach its maximum in 2025 at about 66.5 per cent of the total population. By 2058, the older population is predicted to be larger than the young, with a rate of increase faster than declines.
Madame Speaker, we are experiencing demographic transition and public health must be prepared to respond.
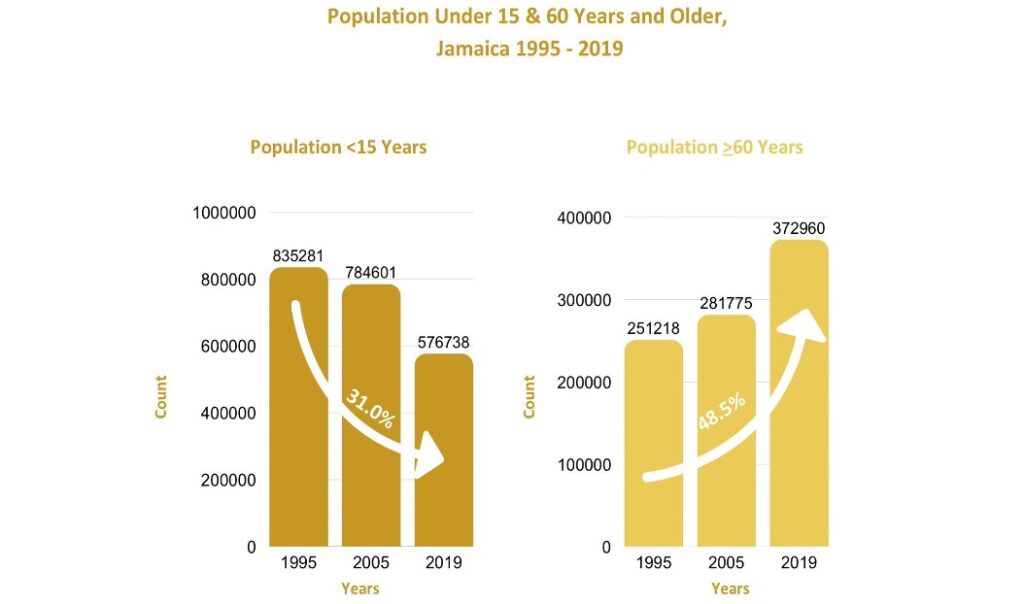
This shift underscores the need to prepare for an ageing population and adapt societal structures, including the workforce and healthcare systems, to address the evolving demographic landscape.
We are developing The Health Programme for Older Persons plan with the following objectives:
- To maximise the period in which older persons maintain good health, wellness, and functional independence through the promotion of healthy ageing throughout the life course.
- To build the capacity of at least 90% of healthcare practitioners in primary care to identify and manage healthcare needs in older adults.
- To provide allied health and rehabilitative services to older persons with complex health and disability needs.
To this end, under the primary health care reform model, we will roll out the training of health care providers this year so that over the next two years we can establish basic screening for functional capacity as part of core services.
We will establish clinics for more detailed assessments and the development of personalised care plans and care pathways to ensure that the older person maximises their potential.
We are expanding rehabilitative and palliative care services in primary care and over the next two years, we intend to establish at least three physiotherapy sites in primary care in the first phase. This will allow easier access for older persons with chronic illnesses like stroke and other disorders that affect mobility.

Madame Speaker, in 2019, we started the Neuropsychiatry Clinic at the Kingston Public Hospital to manage clients with mental disorders caused by brain dysfunction such as Dementia. This plan is now to expand Neuropsych Clinic Services through telehealth, providing case conferences, especially for rural areas.
Madame Speaker, at the same time that we are expanding our family health programmes to include older persons’ health, we are also turning our attention to women’s health to address some specific challenges faced by our women.
The perimenopausal period is one of those issues that affects the well-being and productivity of women. More focus will be placed this year on exploring availability and access to wholistic management in the public sector. This will be addressed first through increasing knowledge and awareness among healthcare workers and equipping them to educate the public at the primary care visits.
Menopause, we know, Madam Speaker, is neither a disease nor a disorder. However, it impacts the state of mind and overall wellness of so many of our women, some of whom begin to experience symptoms as early as in their thirties. A study by the British Menopausal Society notes that more than 80% of women will be menopausal by age 54 with up 80-90% of women having symptoms, 25% of which will be described as severe and debilitating.
There is also growing evidence that there should be a clinical response to this personal life stage experience. I have, therefore, asked a team headed by The Most Hon. Denise Eldemire Shearer, to explore and establish a standard clinical response for this life stage. It is time to recognise that our women experiencing these symptoms deserve our support as a society.
Older men are also an important focus within the Ministry’s health care delivery framework. As men age, they undergo hormonal changes — particularly a gradual decline in testosterone levels — which, although distinct from the hormonal transitions experienced by women, can nonetheless lead to a range of physical, sexual, and psychological health challenges. These may include fatigue, decreased libido, mood changes, and reduced muscle mass.
Recognising and addressing these issues is essential to promoting the well-being and quality of life of older men. As such, their specific health needs will also form a part of the Ministry’s overall strategy to offer comprehensive care for the ageing population, through the adoption of the life course approach.
Mental health

Madam Speaker, across Jamaica, mental illness has been a source of stigma and misunderstanding. We have, however, begun to chip away at entrenched stigma, deepen public understanding and confront the culture of silence that too often surrounds mental health.
In just the last six years, we have taken several significant steps to improve access to and the quality of mental health services.
- We added 14 buses to the Community Mental Health Service, improving mobility and outreach.
- We expanded training for psychiatric nursing aides, enhancing frontline capacity.
- We created 15 new posts for general psychiatrists, child psychiatrists and psychologists, strengthening the human resources in mental healthcare.
- We also launched the Ministry’s Mental Health & Suicide Prevention Helpline, 888-NEW-LIFE. In its first year, the line received 888 calls. By 2024, that number grew to 2,944, a near 70 per cent (69.84%) rise, reflecting growing public engagement and demand.
These improvements have been complemented by other key initiatives:
- The School Mental Health Literacy Programme and Problem Management Plus were introduced to support emotional well-being in communities, promote awareness, reduce stigma and encourage help-seeking behaviours.
- At the Western Child and Adolescent Hospital, now under construction, there are provisions for two wards dedicated to in-patient psychiatric services, increasing capacity for specialised care.
- In collaboration with the Ministry of National Security and private sector partners, we opened a Wellness Centre for children and adolescents in Western Jamaica.
However, the impact of COVID-19, which evidence suggests, has seen an increase in mental health challenges, has underscored the need to do more. Globally and locally, there has been a marked increase in mental health challenges. In response, we must continue to build and sustain an enabling environment, one that protects mental wellness, ensures access to care and furthers public understanding while dismantling stigma.
We see signs of progress:
- The number of people seeking help through our mental health clinics has steadily increased—from 107,837 visits in 2015, to 167,068 in 2019, and 190,598 in 2021.
- The Mental Health & Suicide Prevention Helpline saw a substantial rise in usage, as mentioned earlier.
- Our Do Your Share Mental Wellness Campaign has, in the past 18 months, donated 20 Wellness Benches to promote safe spaces for dialogue and healing, with demand for more growing across the country.
- We also launched the Wellness Check-In Initiative, particularly in schools, providing students with early mental health support and increasing awareness of available resources.
Yet challenges remain. Chief among them are the high attrition rates among mental health professionals and a paucity of needed allied health workers, who are key to comprehensive care and rehabilitation.
Madam Speaker, in the months ahead, the Ministry will therefore take the following actions:
- Fill vacant psychiatric posts to improve service coverage.
- Expand Community Mental Health Service with the addition of mental health officers and psychiatric nursing aides.
- Establish Psychiatric Emergency and Maintenance Teams in selected urban centres to improve response times during crises.
- Develop a National Mental Health Policy to shape the sector’s future.
- Strengthen Mental Health and Psychosocial Support teams for disaster response and humanitarian emergencies.
The Ministry of Health & Wellness is also collaborating with the University of the West Indies to train occupational therapists, one of the critical allied professionals needed to support recovery, rehabilitation and reintegration for persons living with mental illness.
Madam Speaker, the progress is real, but so is the need. We must remain steadfast in our commitment to a mental health service that is accessible, responsive, and compassionate. Together, we can build a Jamaica where mental wellness is a right, not a privilege, and where no one has to suffer in silence.
Maternal health

The Ministry of Health & Wellness continues to advance a coordinated and strategic response to reduce preventable maternal and neonatal deaths in Jamaica. Through strengthened governance and targeted investments, the Maternal and Neonatal Health Programme has made significant progress in improving outcomes for mothers and newborns.
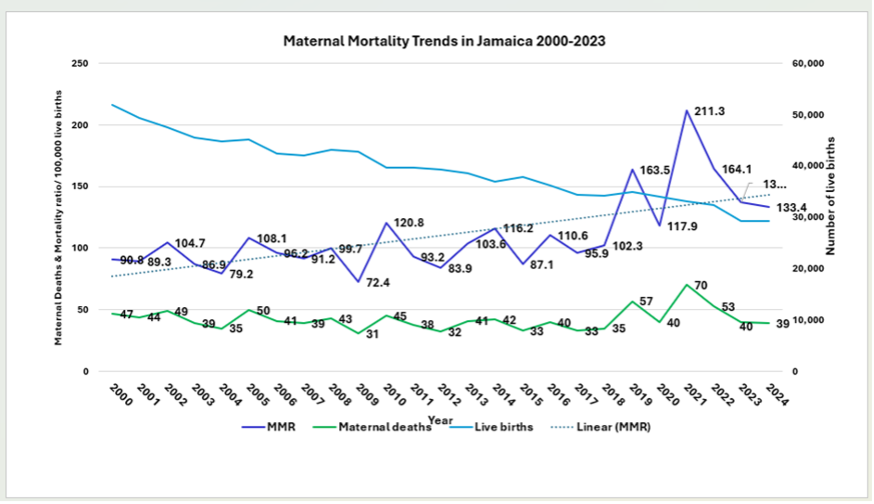
With the Sustainable Development Goal target of 70 maternal deaths per 100,000 live births, an upward trend in the maternal mortality ratio for Jamaica over the past two decades has been a major concern. In 2024, Jamaica recorded a preliminary maternal mortality ratio of 133 per 100,000 live births, reflecting a downward trend post the COVID-19 pandemic from 211.3 per 100,000 live births at the peak of the pandemic in 2021. For the last three consecutive years, there has been a consistent decrease in the rate and with the numbers so far for this year, we are expecting a continued downward trend.
With improved engagement of mothers early in pregnancy, improved governance, improved facilities, improved guidelines and implementation of standards across the country, the Ministry is continuously working to keep the trajectory of the maternal mortality rates at a downward trend.
More than 320 health centres, many of which have undergone recent renovation, offer maternal and child health services.
- There was a marked improvement in the proportion of women who sought antenatal care in the first trimester, reflecting early engagement and equitable access.
- In 2023, 45% of women received antenatal care in the first trimester compared with 22% in 2018. Approximately 99% of pregnant women were attended to by skilled birth personnel.
- Recognising the vulnerability of adolescents, Jamaica launched a dedicated teenage clinic at the Victoria Jubilee Hospital, the largest maternity hospital in the country and the English-speaking Caribbean.
The Ministry has also made deliberate efforts to enhance public education and awareness in this area, including radio advertisements aired on eight national stations from November 2024 through March 2025; and the distribution of flash drives with key antenatal information to be shared on televisions in the waiting rooms at health facilities.

Meanwhile, during the last year, there were also a series of maternal and child health planning meetings, in addition to four regional maternal health fora. These meetings reflect continuous engagement with the service delivery sites and a concentrated national effort to improve standards for responsive comprehensive care in the perinatal period.
- Eight emergency obstetric guidelines for the clinical management of high-priority conditions in pregnancy were printed and disseminated. Revision of the patient-held Maternal Record Book for continuity of care and the neonatal and maternal health sections of the Family Health Manual was completed.
- In 2024/2025, capacity building was a priority. Three online training sessions were based on updated clinical obstetric guidelines addressing the major causes of maternal mortality in Jamaica (hypertension, obesity, cardiac disease, sickle cell disease, sepsis, and thromboembolism in pregnancy).
- Four maternal and two neonatal workshops were conducted, and Point-of-Care Ultrasound (POCUS) training was continued in partnership with the Jamaicans Abroad Helping Jamaicans At Home (JAHJAH) Foundation. Additional simulation-based sessions for postpartum haemorrhage, reinforcing the CODE RED team approach, were conducted.
- The 4th National Perinatal Review was conducted in November 2024. Additionally, monitoring and evaluation tools were developed, including templates for neonatal quarterly reporting to the national level and a postpartum home visits guidance tool. Quality assurance was also prioritised through data validation and the development of a Neonatal Quality-of-Care Audit Tool.
TABLE: Maternal Mortality Trends in Jamaica: 2000-2024
EMTCT for HIV and Syphilis
Jamaica has achieved the elimination of mother-to-child transmission (EMTCT) of HIV and syphilis. This milestone was celebrated on May 7, 2024, along with Belize and St. Vincent and the Grenadines, making them the latest countries in the Americas to receive WHO certification for EMTCT.
AI Technology & the future
Madam Speaker, as we build out our health infrastructure for the future needs of our population, we must continue to vision, forecast and plan for the new and emerging opportunities to improve health service delivery. Leadership requires a futuristic examination of both the challenges we will face and the solutions for those challenges.
The future risk to our health will continue to be lifestyle disease (NCDs). A crude breakout of lifestyle diseases shows more than 80 percent of our population who die each year are dying from NCDs, broken out in general categories of diabetes mellitus, cerebrovascular disease, hypertensive disease, and ischaemic heart disease.
TABLE: Top four causes of death, 2023
| Rank | Cause of Death | Number of Deaths | % of Total Deaths |
| 1 | Diabetes mellitus | 2,618 | 12.0% |
| 2 | Cerebrovascular disease | 2,591 | 11.8% |
| 3 | Hypertensive diseases | 1,725 | 7.9% |
| 4 | Ischaemic heart disease | 1,539 | 7.0% |
| Total Deaths | 21,989 | 38.7% |
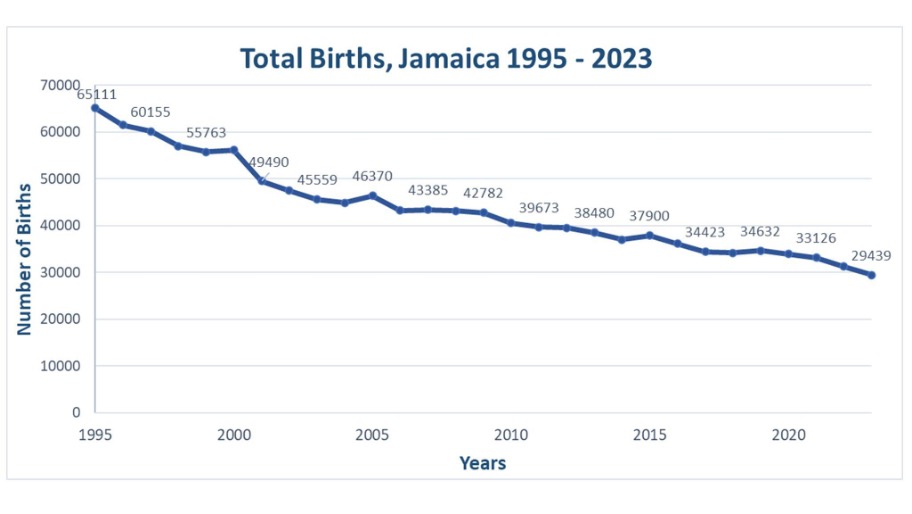
It is also likely that we will continue to see stagnant or lower births.
We will also likely see greater outward and inward migration and a need for greater collaboration between friendly bilateral and multilateral partners for a more cohesive social and economic development.
What is our health policy response to these likely developments?
There are many but I want to focus on two areas; the four major causes of illness and death and the use of AI technology.
New centres of excellence
The four major causes of premature mortality and early onset of illness require a combination of prevention practices, screening and treatment. Our current reforms to primary and secondary healthcare is an attempt at reducing the risks associated with these areas.
But I think we need to do more to map the trajectory of these illnesses and determine the points of intervention that reduce the risks and support continued expansion is specialised monitoring and care.
Madam Speaker, I have asked a team headed by Professor Trevor Ferguson Chair of the NCD Commission to establish sub-committees with this task force for the development of Centres of Excellence around these four key disease risks, with emphasis on:
- Epidemiological profiling and surveillance;
- Primary prevention and health promotion;
- Integrated and people-centred care models; and
- Policy, governance and multisectoral action.
The terms of reference will include mapping the life course of vulnerable groups and determining a pathway to continued research and treatment for these diseases. I have asked for a report on this in twelve months.
AI-Tech Council of Experts
Madam Speaker, this leads me to what I consider to be a most important forward-thinking thrust to secure the future of our health services delivery, under a new thrust called – Artificial Intelligence Technology Enhanced Care for Health (AI-TECH).
Madam Speaker, we have to prepare ourselves for the changes in medical sciences and technology linked to treatment and care to make healthcare screening and treatment more accessible and outcomes more predictable. This is where AI-TECH comes in.
Artificial Intelligence is the process of using technology-driven data to assess, analyse, predict and influence outcomes. In healthcare, easier and faster screening, more minimal invasive treatment procedures and remote monitoring and support for the chronically ill.
Today, Madam Speaker, I am announcing a AI-TECH Council of Experts chaired by Dr. Rubin Pillay, Professor and Assistant Dean of the School of Medicine & Health Innovations at the University of Alabama in the USA to examine the trends and recommend new systems utilising AI technology to address the following areas:
- Cross border treatment support, including with radiology services;
- Lifestyle-linked medical profile predictability;
- Community-based Screening;
- Homecare for the chronically ill and ageing;
- Ongoing monitoring and assessment;
- Any other new trends and practices ethically acceptable for healthcare delivery.
This AI-TECH Council of Experts will conduct the necessary applied research and coordination to generate a report aligned to the country’s ten-year strategic plan to integrate AI technology into our health services delivery.
I have asked the NHF to provide an initial J$30M to support a secretariat for this work which I have asked to be done over a twelve-month period, culminating in a one-day workshop in Jamaica where the report will be presented and discussed by a cross-section of health and health-related stakeholders.
My expectation is that the report will contain practical, implementable solutions for policy considerations, which will be taken to the cabinet for its consideration and eventual implementation.
I have also tasked the Wellness Fund to consider for the next research cycle that is focused on technology-driven healthcare to hopefully bolster the offerings for a better-delivered healthcare system.
The goal, Madam Speaker, is to make best use of Artificial Intelligence in healthcare, including in the area of screening, self-monitoring and remote access to treatment. The future requires us to carefully consider and prepare for what we do with AI in medicine, guided by science.
Madam Speaker, the future of healthcare is with AI-TECH! This Government will get it done. We must stay the course!
Conclusion

After nine years as Health and Wellness Minister, under this Andrew Holness led administration, I am proud of the team that has led this country through a series of crises while still building out our health infrastructure like no other administration before; reviewing and reforming for better policies, while preparing for the future challenges of healthcare.
We managed the tail end of the Zika virus, then Chick V, one year of a dengue outbreak, then the dreaded COVID-19 pandemic and the collapse of the long neglected CRH.
In all this, we have remained steadfast, not panicking or surrendering but demonstrating strong and decisive leadership.
While confronting these challenges, we have embarked on the largest infrastructure upgrade of hospitals and health centres and policies that have clearly outlined the way forward for primary healthcare reforms and secondary healthcare reforms; adding more services, more doctors and nurses.
We have started to digitize our health systems, a first in the Caribbean region, for better patient care and management.
We have fixed more health centres than anytime before and offered more services at the community levels and it is paying off with a shift by Jamaicans to the community health centre away from hospitals.
And we have promoted wellness as a lifestyle concept that encourages rest, relaxation, humour and happiness.
In all this, we have eased the burden of many Jamaicans and saved many lives.
Over the last year:
- 4,274 Jamaicans benefited from a Second Chance Smiles, receiving dentures;
- 119 Jamaicans received prosthetic limbs from our New Limb New Life programme;
- 756,001 received free drugs from the NHF;
- 289,430 free screening tests were performed under the Know Your Numbers initiative;
- 1,892,106 visits to our Health Centres;
- 1,154,840 visits to hospitals; and
- 63,562 life-saving surgeries.
And we continue to build out for the next term to bring:
- Some 450 more new beds;
- 27 new operating theatres; as well as
- More diagnostic equipment through our leasing programme
- More drugs from the NHF
- More doctors, more nurses
- More opportunities for training and development and increased benefits to the healthcare team.
I agree, we are not where we want to be, but we are making good progress, and Jamaicans are benefiting more today from public health services, than they were in 2015.
Let’s stay the course! We must stay the course! Lets keep moving!
God Bless Jamaica Land We Love!







Comments